Gastric sleeve surgery is proven to be an effective major weight loss option for people who experience obesity. However, gastric sleeve surgery is just that - a surgery. With any procedure, there are health considerations doctors and surgeons must assess for an individual to be eligible for a sleeve gastrectomy.
While some individuals will be the perfect candidate and will see considerable weight loss results from gastric sleeve surgery, for others, the procedure may not be viable due to medical history, age, or lifestyle.
This article will explore the eligibility criteria for gastric sleeve surgery and what to expect before and after surgery.
BMI Guidelines
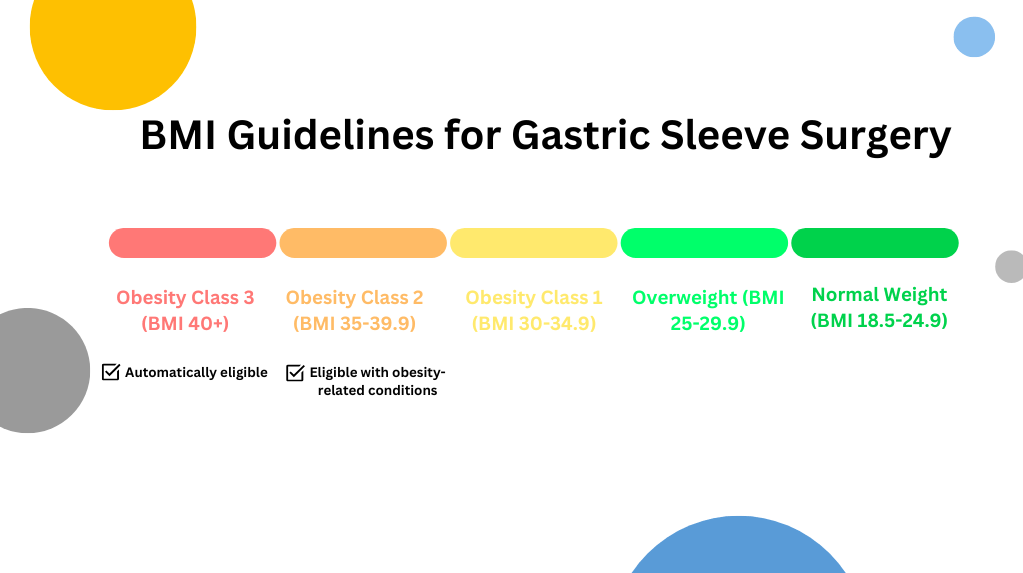
Gastric sleeve surgeons use the BMI scale as a helpful guide to determine whether it is safe and healthy for an individual to receive surgery. Those with a Body Mass Index (BMI) over 40 or a BMI over 35 with an obesity-related disease, like diabetes, hypertension, or sleep apnea, are generally eligible for gastric sleeve surgery.
BMI indicates an individual's body size, calculated by weight and height. The BMI scale begins at 20 to 24.9 (normal range) and spans 50+ (super obese). It’s important to note that the BMI scale is used as a guideline – this means that individuals below with a BMI below 35 but have struggled with weight-related health concerns throughout their lives, may be eligible for gastric sleeve surgery.
Health Guidelines
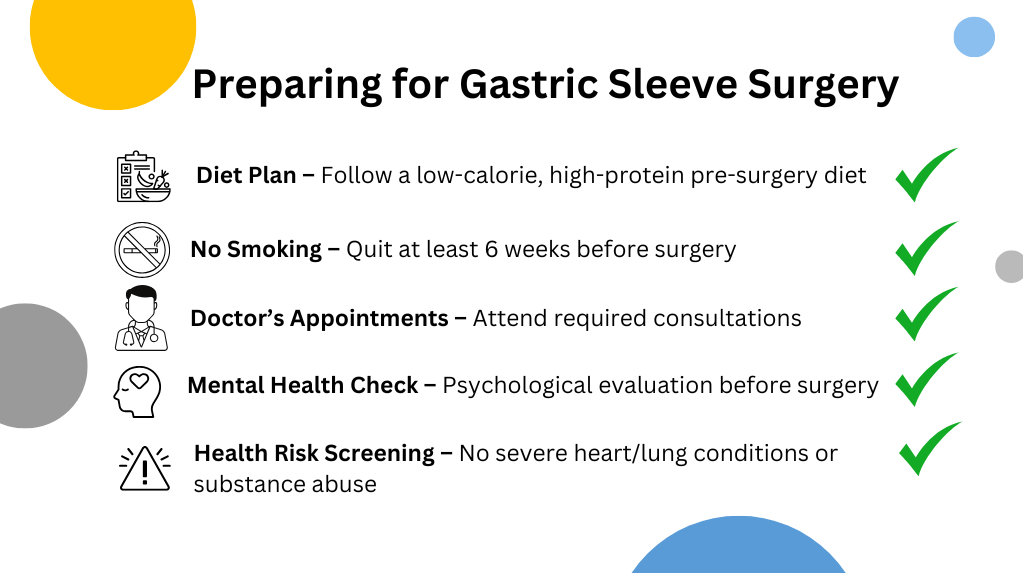
To qualify for gastric sleeve surgery, individuals must meet the doctor's or surgeon's health guidelines. For example, they may be required to attend information sessions about the surgery or have their physical and mental health tested through meetings with dietitians or psychologists.
Bariatric surgeons will also assess an individual's health risk factors that may impact the surgery and the person's overall well-being. The most common health risk factors that can disqualify someone from gastric sleeve surgery include severe lung or heart diseases, alcohol or drug addictions, problems with the stomach, oesophagus, or intestine, autoimmune diseases, and blood disorders. Individuals must also be between the ages of 16 and 75 and not pregnant.
Lifestyle & General Readiness
To get the most out of the surgery, individuals should start making lifestyle changes in the lead-up to gastric sleeve surgery. Diet is the biggest lifestyle change for the surgery. In fact, your physician will also refer you to a dietitian who will provide a pre-surgery diet plan. Every diet plan is unique to each individual but will generally aim to reduce calories, maximise protein intake, include healthy fats, and stay hydrated.
If you’re a smoker, you’ll be required to quit at least 6 weeks before the surgery or as stated by your doctor. Smoking affects the immune system and will negatively impact your healing and recovery period post-surgery – increasing the risk of complications.
What to Expect After Surgery
After surgery, you may have to stay in the hospital for 1 to 3 nights after gastric sleeve surgery, but your recovery will continue for up to 2 to 3 weeks post-surgery. You may feel some discomfort and difficulty moving around, so you may need to take pain medication in the short term. You will also have regular check-ups and blood tests following the surgery.
The first week after surgery, you will be consuming clear liquids, like clear broth and decaffeinated and sugar-free drinks. From the second week, you’ll slowly transition to pureed food, before solid foods after a few weeks. Expect to feel fuller much more quickly, so only make small meals and avoid drinking liquids with meals.
Your doctor or surgeon will advise you on healthy lifestyle habits to support gastric sleeve surgery. A week after surgery, you can start physical activity, like walking and light weights, to promote recovery and encourage a healthy lifestyle.
Timelines for Weight Loss
Generally, individuals reach their goal weight loss within 9 to 12 months after surgery. The typical timeline for weight loss is:
1 month
Weight loss is most evident in the first month after gastric sleeve surgery – the average weight loss in the first month is around 2kg per week. The liquid and pureed food in the post-surgery diet will further encourage this weight loss - in a healthy way.
3 months
At 3 months, you can expect to lose an average of 25 to 35% of excess weight. By this point, you will have moved from liquid to solid foods and started engaging in more physical activity.
6 months
By 6 months, most people lose about 45 to 55% of their excess weight. At this stage, it’s normal for weight loss to continue but start to slow down. You should continue to see noticeable results in your weight loss by following your diet plan and exercising regularly.
1 year
At the one-year mark, you should be close to your goal weight. Generally, weight loss patients will lose an average of 65 to 75% of their excess body weight and see significant improvements in their weight-related health complications.
18 months and over
The rate in which weight is lost will begin to plateau at the 18 month mark. However, the goal from here should not be to keep losing weight (if you’ve hit your goals!), but to keep the weight off in a healthy, sustainable way.
